Online available: 2025-07-01
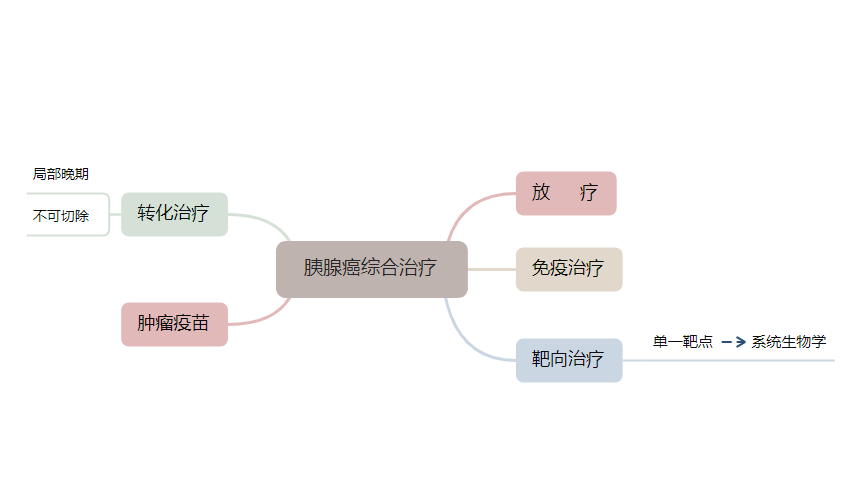
Pancreatic cancer is among the most lethal malignancies of the digestive system, with an overall 5-year survival rate of only 13%. In recent years, advances in tumor molecular biology have shifted therapeutic strategies from a “one-size-fits-all” approach to molecular subtype-based, targeted, and personalized therapies. Concurrently, the widespread implementation of multidisciplinary team (MDT) collaboration and full-cycle patient management has optimized the comprehensive treatment paradigm, aiming to balance undertreatment and overtreatment. However, the high heterogeneity of pancreatic cancer, limited availability of targeted approaches for key driver genes, intrinsic and acquired resistance mechanisms, and the immunosuppressive tumor microenvironment continue to significantly hinder the advancement of precision molecular classification and individualized treatment, leading to no substantial improvement in patient prognosis to date and enormous challenges in clinical diagnosis and treatment. Current research indicates correlations between molecular subtypes (including classical, basal-like, quasi-mesenchymal, and squamous) and clinical phenotypes. Liquid biopsy technologies—such as circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and exosomes—are being explored for early diagnosis and real-time disease monitoring. In targeted therapy, research is centered on KRAS and resistance mechanisms. Immunotherapy must overcome the challenges of low immunogenicity and an immunosuppressive tumor microenvironment, with various combination strategies undergoing clinical investigation. Artificial intelligence (AI) and big data are expected to enhance diagnostic imaging, molecular subtyping, and intraoperative navigation. Future directions should focus on strengthening interdisciplinary collaboration and integrating molecular classification, targeted and immunotherapeutic strategies, and AI technology to realize precision, comprehensive treatment for pancreatic cancer.